Friday, 16 September 2022
37 year old male, chronic alcoholic with SOB and anasarca
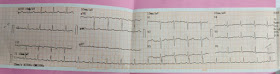
A 51 yr old man with loss of sensation in left foot
13th Sep,2022
This is an online E log book to discuss our patient's de-identified health data shared after taking his/her/guardian's signed informed consent.
Here we discuss our individual patient's problems through series of inputs from available global online community of experts with an aim to solve those patient's clinical problems with collective current best evidence based inputs.
This E log book also reflects my patient-centered online learning portfolio and your valuable inputs on the comment .
K. Chetana
Roll no. 74
A 51 yr old male patient farmer by occupation resident of West Bengal presented to opd with chief complaints of decreased sensation on left foot since 3 years, swelling of foot since 3 yrs and ulcer since 10 months.
HISTORY OF PRESENTING ILLNESS-
Patient was apparently asymptomatic 25 yrs ago. Then on a regular football match his left ankle was twisted because he fell into a ditch and had swelling over the ankle without any other skin changes. He was taken to local general hospital and there he was given few medications and he continued his work as usual and the swelling subsided within 1-2 weeks. Then again after 4 yrs (I.e 21 yrs ago) he fell into the pit while playing football and twisted the same ankle and had to go the hospital and was given medication and so this time too there was no more of skin changes and no limitation to work and swelling subsided within 2-3 weeks.
Then 18 yrs later (I.e 3 yrs ago) he was on a morning walk where because of darkness he couldn't see and fell down again and was taken to orthopedic where on x rays he was found to be having a fracture on the 5th metatarsal and he was advised for an open reduction but the patient denied surgery because of his financial condition and so was given tablets. According to patient he was able to walk during the time he had fracture and would continue doing his work with reduced workload. He could not dorsi flex his leg.After 4-5 months of this episode and a serial x rays his fractured appeared healed.
03-01-2019-
But slowly around that time he started to loose sensations in the lateral aspect of his foot which over the time progressed to medial side and now he has no sensation down below the ankle of his left foot.
He had swelling in his left foot since then. Back in Nov 2021 he noticed a small ulcer on his sole on left foot on the medial side.Ulcer characteristics?.He has no idea of any known trauma there. In the due course of time the depth of ulcer increased and in the month of may 2022 it was nearly 2-4 cm deep. He is farmer and works bare foot in the fields and everyday his ulcer would fill with mud and he would just simply wipe it off as he had no sensation there. But as the depth had increased he visited the local hospital in the may where he was given a cream to be applied once a week and was asked not to work more in farms.
He applied the cream for 3 weeks (I.e 3 times) and seeing no change in the ulcer depth he went back to hospital where again he was given some tablets and advised to wear an orthopedic shoe. But just after wearing it for 10-15 mins he had a bleed on the back of his foot and he did not wear it again. He was not able to feel that he was bleeding there until he was told by his wife. There is also a known incident where his left foot had a fire spark nd he still didn't know until somebody else around him mentioned.
His ulcer size reduced but still it is present and he came to our hospital because of his decreased sensation in the left foot and swelling.
Previous hospital visit report-
PAST HISTORY-
Not a known case of diabetes, hypertension, asthma, leprosy, thyroid, epilepsy.
FAMILY HISTORY-
No known family history.
PERSONAL HISTORY-
Diet Mixed
Appetite Normal
Sleep Adequate
Bladder and bowel Regular
Allergies None
Addictions- Tobacco 10 gm / 3 days since 20 yrs.
Daily routine- He is a active person doing all his activities. His occupation involves him working in watery soil but since this may he is not indulging much in water works.
GENERAL EXAMINATION-
Patient is conscious coherent and co operative well oriented to time place and person.He is moderately built and nourished.
Patient was examined in a well lit room and consent was taken.
Vitals -
PR-78 bpm
BP- 130/80
RR-16cpm
SPo2- 99 ra
Temp-Afebrile
Pallor - Absent
Icterus - absent
Clubbing - Absent
Cyanosis- Absent
Lymphadenooathy- absent
Edema - on left foot non pitting type
Clinical pictures?of ulcer /edema of leg
SYSTEMIC EXAMINATION-
CVS-
S1, S2 heard
No murmurs.
RESPIRATORY-
Non vesicular breath sounds
Trachea central.
No wheeze.
ABDOMEN-
Soft and non tender.
CNS-
Gait- Equine Gait