THIS IS AN ONLINE E LOG BOOK TO DISCUSS OUR PATIENT'S DE - IDENTIFIED HEALTH DATA SHARED AFTER TAKING HIS / HER /GUARDIAN'S SIGNED INFORMED CONSENT .HERE WE DISCUSS OUR INDIVIDUAL PATIENT'S PROBLEMS THROUGH SERIES OF INPUTS FROM AVAILABLE GLOBAL ONLINE COMMUNITY OF EXPERTS WITH AN AIM TO SOLVE THOSE CLINICAL PROBLEMS WITH COLLECTIVE CURRENT BEST EVIDENCE BASED INPUT.
This E blog also reflects my patient centered online learning portfolio and your valuable inputs on the comment box is welcome.
I have been given this case to solve in an attempt to understand the topic of " patient clinical data analysis" to develop my competency in reading and comprehending clinical data including history, clinical findings, investigations and come up with diagnosis and treatment plan
23-08-2022
A 28 year old male came to OPD with cheif complaints of abdminal distention since 25 days and breathlessness since 5 days
HOPI:
23-08-2022
A 28 year old male came to OPD with chief complaints of
Abdominal distention since 20 days
Shortness of breath since 15 days
History of present illness
Patient was apparently asyptomatic 4 months back then In April he had fever ,yellowish discoloration of eyes for 3 days , fever is not associated with chills and rigor ,no evening rise of temperature he went to hospital , used medication for 1week.
Symptoms subsided after a week ,he started to consume alcohol(180 ml) daily since then .
In the month of June he had Abdominal distension, yellowish decolorisation of sclera , went to a hospital in jangaon took ayurvedic medicine for 1 week , symptoms subsided.
He started to drink alcohol from July 1st till 27 th July .
Then he presented on July 28 with complains of Abdominal distension since 6days, Shortness of Breath Gradelll ,fever not associated with Chills and rigor without evening rise of temperature, Altered sleep cycle,facial puffiness,, pedal edema is seen for 3 days.
On 29/7 Ascitic tap was done.
22-08-2022
The patient came back to OPD with abdominal distention since 20 days that increased on consuming food and decreased on passing stools
The patient also complains of shortness of breath since 15 days even while resting associated with palpitations , giddiness and fearfulness
He developed dry cough since 5 days that relived on medication
He complains a fever episode 2 days ago that relived on medication
Patient has loss of appetite since 2 days due to abdominal tightness
Past history
N/K/C/O DM/HTN/TB/ASTHMA/CAD
PERSONAL HISTORY:
Diet : Mixed
Appetite : Decreased
Sleep : Disturbed
Bowel and Bladder moments : Constipation is seen
Micturition : Normal
FAMILY HISTORY:
Not significant
General physical examination:
Patient is conscious ,coherent and cooperative and well oriented to time, place and person.
moderately built and nourished.
Pallor-absent
Icterus-present
Cyanosis-absent
Clubbing-absent
Lymphadenopathy-absent
Edema-absent
Vitals:
Temperature - 98.2*c
PR :- 95bpm
RR :-22cpm
BP :- 130/80mm Hg
SPO2 :- 98%
GRBS :- 167mg/dl.
Systemic examination:
CVS- S1S2 no murmurs
RS-BVS+, wheeze+
P/A-soft
Uniformly distended.
Umbilicus everted.
Engorged veins present.
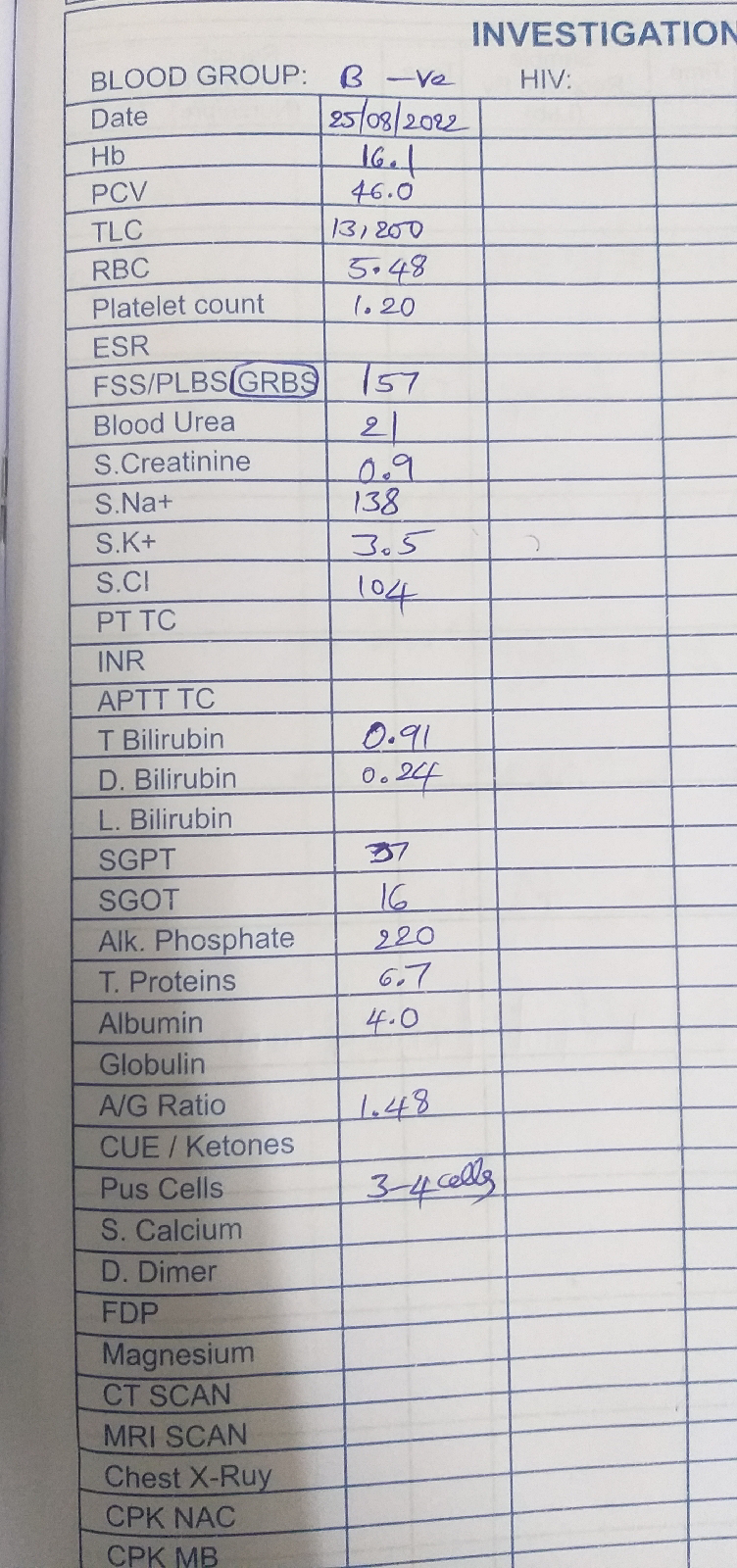
Investigations:
LFT:
ECG:
USG:
2D ECHO:
X-RAY:
PROVISIONAL DIAGNOSIS:
Chronic liver disease
Treatment:
1. FLUID RESTRICTION.
2. SALT RESTRICTED NORMAL DIET.
3. INJ. CEFOTAXIM 2 GRAM TWICE DAILY INTRAVENOUSLY.
4. INJ. VIT K 1 AMP IN 100 ML NS ONCE DAILY INTRAVENOUSLY.
5. INJ. THIAMINE 1 AMP IN 100 ML NS ONCE DAILY INTRAVENOUSLY.
6. INJ. PAN 40 MG TWICE DAILY INTRAVENOUSLY.
7. INJ. ZOFER 4 MG THRICE DAILY INTRAVENOUSLY.
8. TAB. PCM 650 mg SOS (<1 GRAM / DAY).
9. SYP. LACTULOSE 15 ML 30 MINUTES BEFORE FOOD THRICE DAILY.